Non responsive and refractory coeliac disease
Most people feel better after starting the gluten free diet, however around 30% of people may experience ongoing symptoms. In most cases, the reason people don’t feel better after starting a gluten free diet is because they are still eating foods containing gluten without knowing it. If you're unsure about which foods you can include on your gluten free diet, our Helpline team might be able to help, so call us on 0333 332 2033.
 Some people with coeliac disease do not respond to the gluten free diet or may initially respond to the diet and then start to experience symptoms again. This is called non responsive or refractory coeliac disease. If you have ongoing symptoms, there are specialists who can help.
Some people with coeliac disease do not respond to the gluten free diet or may initially respond to the diet and then start to experience symptoms again. This is called non responsive or refractory coeliac disease. If you have ongoing symptoms, there are specialists who can help.
Teams led by Prof David Sanders in Sheffield and Dr Jeremy Woodward in Cambridge have been approved by the NHS for a Rare Disease Collaborative Network (RDCN) to provide support with the diagnosis and care of people with non responsive or refractory coeliac disease.
The first step for people with suspected non responsive coeliac disease is to confirm the original diagnosis of coeliac disease, followed by a repeat endoscopy with biopsies. You can start this process with a visit to your GP to ask for a referral. The repeat endoscopy with biopsies will help to determine if you have persisting gut damage which will then help guide the next steps.
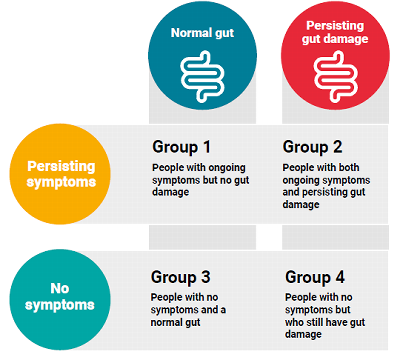
If you have no gut damage but are still having symptoms, other causes of your symptoms will be considered. For example irritable bowel syndrome or lactose intolerance.
If you have persisting gut damage and are having symptoms, your diet will be reviewed to make sure there is no accidental gluten exposure. Your healthcare team will also consider other causes including "super sensitivity", slow response to treatment and refractory coeliac disease. Adherence to the gluten free diet varies from 42 - 91% and gluten exposure is the most common cause of ongoing symptoms. During the dietary review, the dietitian may discuss avoiding certain foods which may be causing sensitivity.
If you have no symptoms but your biopsies show persisting gut damage, your doctor will explain the ongoing inflammation with you and the risks of long term complications. You may also be referred to a dietitian for more support with your diet.
If you don't have any symptoms and you have no gut damage, you'll be referred back to your GP for annual review.
Refractory coeliac disease
Refractory coeliac disease (RCD) is a very rare complication of coeliac disease with an increased risk of certain types of cancer. RCD is reported to affect between 0.3 to 4.0% of people with coeliac disease. It is likely to be over diagnosed because of the difficulties in differentiating between ongoing gluten exposure, people who are "super sensitive" and true RCD.
There are two types of RCD, type 1 and type 2. These types are different from each other in the way they are diagnosed and the symptoms that they cause.
Special techniques for the diagnosis of RCD (immunohistochemistry and flow cytometry) are offered at the Cambridge and Sheffield specialist centres. Another type of testing, called clonality testing is available elsewhere but it isn't enough to conclusively diagnose RCD type 2.
Treatment
Because refractory coeliac disease is so rare, there have been limited studies on it. In addition to the gluten free diet, drug treatments may be needed such as steroids, immunosuppressive drugs, chemotherapy or a combination of these.
The treatment chosen will need to be closely monitored by the specialist healthcare team.
Even if you are not responding to the gluten free diet, it’s essential that you continue to follow a strict gluten free diet to prevent further ongoing symptoms and future complications.
Regular reviews with your dietitian are important to make sure that you’re getting all the nutrients that you need and that your diet is well balanced.
Complications
RCD type 2 can progress to a form of gut cancer known as enteropathy associated T-cell lymphoma (EATL) in around three to seven out of ten cases. In contrast, RCD type 1 rarely progresses to EATL. Therefore it is really important to have the correct diagnosis and treatment.
Cases of cancer are very rare, so if you're experiencing ongoing symptoms don't panic and speak with your healthcare team.
What should I do if I'm having ongoing symptoms?
Anyone experiencing or concerned about symptoms while following a gluten free diet should speak with their healthcare team. Symptoms are most likely due to eating gluten accidentally, but if not the specialist teams in Cambridge and Sheffield are there to support your local healthcare team if needed.
We have developed downloadable Fact Sheet to support you and your healthcare team.