Rasmus, Lene and Ida B cells
B cells are responsible for producing antibodies. In coeliac disease, B cells produce antibodies to transglutaminase 2 (TG2) an enzyme that is present in the body itself. These antibodies are tightly linked to coeliac disease, indicating that B cells are important players in disease development. The antibodies themselves, however, are not known to cause disease. We are therefore interested in exploring alternative functions of B cells to understand their role in coeliac disease.
TG2 specific B cells can present gluten to gluten specific T cells
 My name is Rasmus Iversen and I am a researcher at the Department of Immunology. My main research focus is to understand how antibodies and B cells that react against transglutaminase 2 are involved in the development of coeliac disease. Our approach relies on isolation and characterisation of molecules and cells from biological samples donated by patients.
My name is Rasmus Iversen and I am a researcher at the Department of Immunology. My main research focus is to understand how antibodies and B cells that react against transglutaminase 2 are involved in the development of coeliac disease. Our approach relies on isolation and characterisation of molecules and cells from biological samples donated by patients.
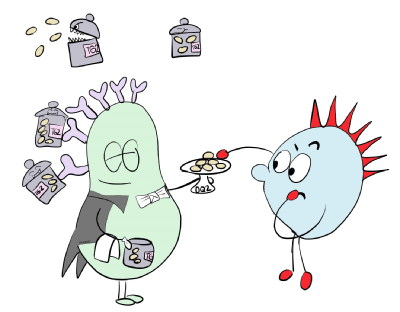
The T cell and B cell “handshake”
Yesterday, Asbjørn and Louise presented T cells as a key cell type of the immune system causing coeliac disease. T cells are dependent on receiving signals from other cell types and can only recognise gluten when fragments are presented on HLA-DQ2 or HLA-DQ8. Our recent findings suggest that B cells can be involved in presenting the gluten fragments to T cells and that this contact between T cells and B cells may drive disease development. The outcome of this “handshake” between T cells and B cells is mutual activation of both cell types, leading to release of molecules that cause inflammation from the T cells as well as antibody production by the B cells. This model can explain the link between coeliac disease and antibodies against transglutaminase 2.
Different flavours of B cells and antibodies
 By studying the antibodies produced by B cells, we have discovered that not all antibodies to transglutaminase 2 are the same, since they can attach to different parts of the protein. Many of the antibodies bind preferred areas on the transglutaminase 2 surface, and the B cells that make such antibodies are best at stimulating T cells. We have also seen that production of these antibodies occurs with the onset of coeliac disease and tissue damage in the gut. Based on our results, we believe that you need to engage certain types of immune cells, both on the T cell and B cell side, to develop coeliac disease. The potential for targeting such cells with therapeutics may open new possibilities for treatment.
By studying the antibodies produced by B cells, we have discovered that not all antibodies to transglutaminase 2 are the same, since they can attach to different parts of the protein. Many of the antibodies bind preferred areas on the transglutaminase 2 surface, and the B cells that make such antibodies are best at stimulating T cells. We have also seen that production of these antibodies occurs with the onset of coeliac disease and tissue damage in the gut. Based on our results, we believe that you need to engage certain types of immune cells, both on the T cell and B cell side, to develop coeliac disease. The potential for targeting such cells with therapeutics may open new possibilities for treatment.
B cells go through several developmental stages before they start making antibodies. We are currently trying to characterise all of these stages in order to understand how the antibody production starts and where T cells and B cells meet. At the final stage, B cells accumulate as so called plasma cells that sit in the gut wall and produce large amounts of antibody.
Plasma cells do more than secrete antibodies
 We are Lene Høydahl and Ida Lindeman, a Postdoc and PhD student working in Ludvig Sollid’s group. Our research interest is the late stage B cells, called plasma cells, which produce antibodies against transglutaminase 2 and gluten in people with coeliac disease. Specifically, we are interested in understanding if and how plasma cells contribute to coeliac disease - we suspect that plasma cells have other functions besides antibody production!
We are Lene Høydahl and Ida Lindeman, a Postdoc and PhD student working in Ludvig Sollid’s group. Our research interest is the late stage B cells, called plasma cells, which produce antibodies against transglutaminase 2 and gluten in people with coeliac disease. Specifically, we are interested in understanding if and how plasma cells contribute to coeliac disease - we suspect that plasma cells have other functions besides antibody production!
To learn more about these cells, we have isolated and analysed plasma cells from gut biopsies of people with coeliac disease and studied their transcriptomic profile (ie which genes they express) and which molecules they have on their cell surface. This gives us important clues about their function.
Ida has performed the transcriptomic analyses and seen that plasma cells express genes coding for HLA molecules, including HLA-DQ2. Plasma cells also express genes coding for signal molecules that can be expressed on the cell surface or secreted from the cells.
Lene has studied cell surface expression of some of these molecules and seen that they are present on the surface of the plasma cells. These studies have shown that the plasma cells do in fact have HLA-DQ2 on their cells surface and that plasma cells are able to present gluten fragments on HLA-DQ2, a prerequisite for talking with T cells. We have also confirmed that the plasma cells express certain “signal” molecules on their cell surface. All these molecules are necessary for an efficient T cell and plasma cell “handshake”.
Our current theory is that plasma cells also act as antigen presenting cells for T cells and that they can be important to keep the T cells activated in the gut in coeliac disease. Our future research will explore this in more in detail. If B cells and plasma cells have important roles as antigen presenting cells in coeliac disease, targeting these cells offers a new potential treatment strategy.